The UCSF Hip Fracture Protocol is an interdisciplinary joint effort among orthopedic surgery, anesthesia, hospital medicine, cardiology, emergency and geriatric medicine. This website summarizes the care pathway for all hip fracture patients admitted to UCSF. These patients will be followed by the Geriatric-Orthopedic Co-management service, regardless of admitting team. It is a resource for residents, service attendings and any other team members to optimize care based on best available evidence. It has been reviewed and approved by the departments and divisions of each service.
Menu
Emergency Department Care
1. In your note use dot phrase: .hipfracture
2. Radiographs
- Low AP pelvis, AP of affected hip, AP and lateral of affected femur
MRI indicated if high suspicion but no clear fracture on x-ray (CT scan if MRI not available)
3. Labs
- CBC, Chem 10, Coags, Vitamin D
- Type and Cross for 2 units pRBCs
- Type and cross for 2 units FFP if patient on warfarin
4. Chest Xray indicated if history of heart or lung problems or new symptoms
5. EKG indicated if history of heart or lung problems or new symptoms
6. Pain Control: All patient should be considered for iliaca fascial block
8. Consults:
- All patients: orthopedics
- 65+: Geriatrics (9am-5pm only) 443-8532
- If after 5pm (or geriatrics unavailable) with acute medical needs: Medicine consult
9. Admit patient to Orthopedics or Medicine and request 7L bed if available
- Patient admitted to Orthopedics unless age > 90, multiple medical co-morbidities requiring active management, or significant active medical issue
- Geriatrics comanges/consults on all patients 70 and older admitted to Parnassus and is available for e-consults for patients admitted to Mount Zion
10. Delirium/agitation Management
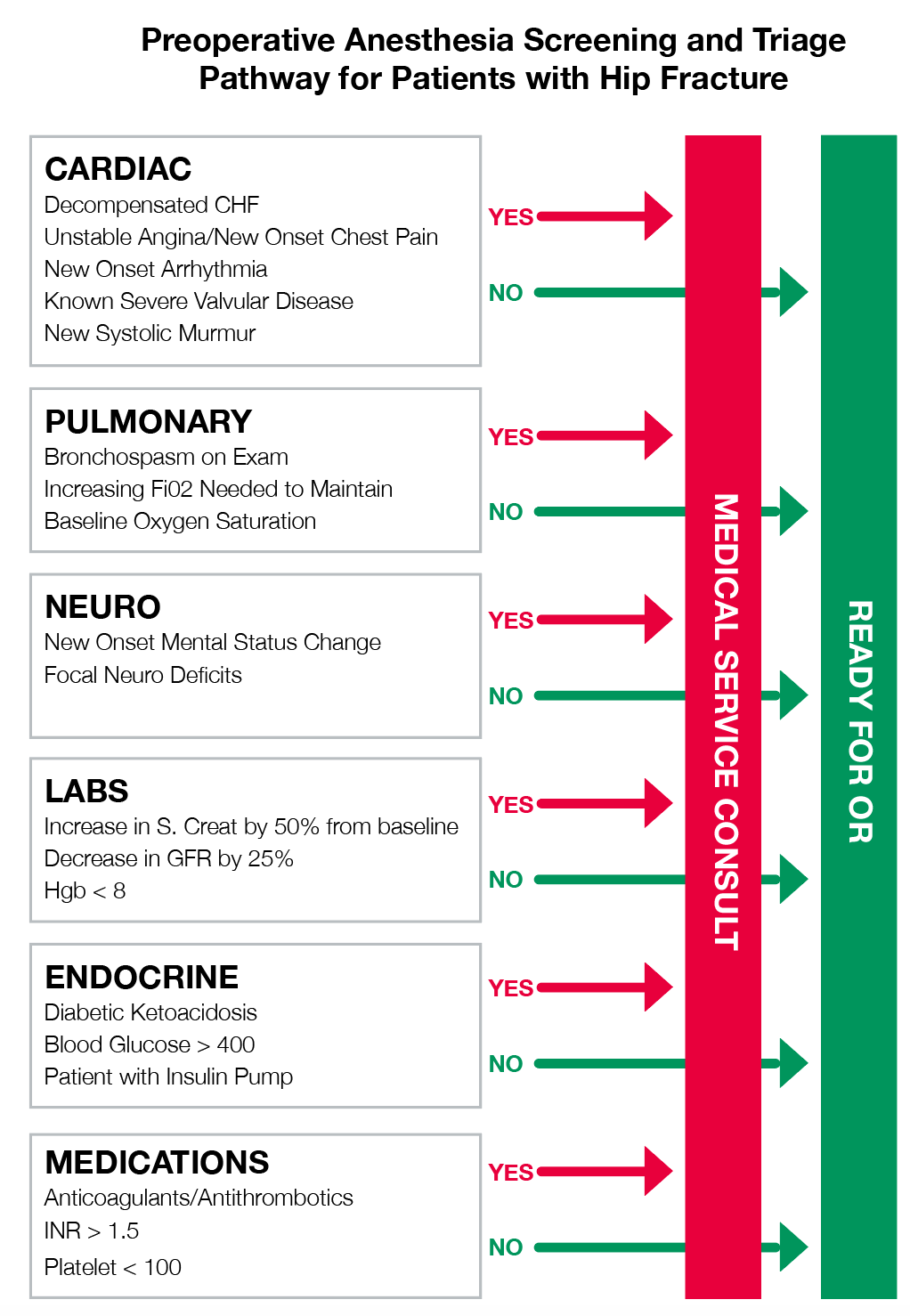
Pre-operative optimization guidelines
Workflow
- Goal time to OR is <24 hours as a hip fracture needs urgent surgical repair. Getting to the OR within 24 hours is associated with improved health outcomes including decreased post-operative complications (pneumonia, hypoxia, arrhythmias, UTIs, PE), lowered mortality, improved pain and decreased rates of delirium shorter length of stay.
- Orthopedic chief discusses all hip fractures admitted overnight or planned for surgery each day with E1 in the morning. This discussion will include any relevant co-morbidities that may affect surgical planning.
- Patients are optimized by 11AM if they present overnight, ASAP if they present during the day, but no later than 11AM the following day
- Orthopedic On-call chief notifies attending on-call and covering trauma attending as well as University Service Chief and Intern (Attending covering case will depend on when case can go to the OR, if case goes from 1PM to 7PM then ortho trauma attending of the day will cover. If the case goes after 7PM or on weekends then general on-call attending will cover).
Medical Optimization
General orders
1. Call Geriatrics or Medicine for any pre-operative optimization needs (only they should determine if another consult, like cardiology, is needed for optimization). Orthopedics is not allowed to call Cardiology without discussing with Geriatrics or Medicine.
2. For patients admitted in the evening keep NPO after Midnight in anticipation of OR next day, for patients admitted in the morning keep NPO for possibility of OR the same day.
3. Start aggressive hydration: 100-150cc/hr normal saline maintenance fluids started early
4. Hold ACE inhibitors to prevent intraoperative hypotension and AKI, restart POD #1
5. Continue beta-blockers/rate control medications
7. Anticoagulation management or reversal
8. Delirium Order Set and delirium prevention
9. PT/OT ordered pre-emptively to service aware of impending need
10. Patient admitted to 7 Long if possible
11. Order Vitamin D if not already done in ED
12. PMD contacted on admission to confirm medication list and co-morbidities (Geri/Med)
Pulmonary Compromise
- COPD/Asthma- continue inhaled bronchodilators/steroids. If acute, serious exacerbation--consider delaying surgery 24-48 hours with steroid treatment
- Acute bronchitis/PNA: Assess for sepsis/SIRS/bactermia and treat as necessary
Anemia
- Transfusion trigger is Hgb < 8
Diabetes/Elevated blood sugar
- Goal blood sugar 100-180 (too low increases falls, too high impedes repair)
Cardiac Anesthesia: Only a requirement at the discretion of the anesthesia service (Medicine, Cardiology, or Geriatrics should NOT recommend)
Swart E, Kates S, McGee S. The Case for Comanagement and Care Pathways for Osteoporotic Patients with Hip Fracture. J Bone Joint Surg. 2018; 100(15):1343-1350.
Only unstable conditions should delay going to the OR (Active ACS, Unstable Arrhythmia, Decompensated CHF, and Known Moderate/Severe Aortic or Mitral stenosis):
1. Active Acute Coronary Syndrome (ischemic EKG changes or elevated troponin)
- Cardiology consult and OR delay until optimized
2. Unstable Arrhythmia (hypotension or significantly uncontrolled)
- Cardiology consult and OR delay until optimized
3. Decompensated CHF
- Severe decompensation with new oxygen requirement or severe symptoms needs an TTE* before OR
4. Known Mod/Severe AS or Mod/Severe MS with no TTE* in past 12 months
*TTEs: Getting a TTE can delay surgery and possibly worsen outcomes. Only patients with the following conditions require a new TTE (a recent TTE is defined as in the last 12 months):
1. CHF with signs of severe decompensation (with new oxygen requirement or severe symptoms)
2. Known Mod/Severe AS or Mod/Severe MS with no echo* in past 12 months
3. New oxygen requirement
*TTEs should be expedited- call cardiology early with plan to be be completed by 11am for surgical decision
Statement to be placed in chart when optimized:
“This surgery is urgent and patient is medically optimized for the proposed procedure and requires no further medical evaluation at this time. Please discuss with anesthesia that spinal anesthesia is preferred if appropriate and safe.”
Pre-operative anticoagulation management/reversal
1. Continue Aspirin at all doses
2. Warfarin
- Hold Warfarin, give Vitamin K 5mg PO x 1 ASAP
- Type and cross for 2 units FFP
- Goal INR for OR is 1.5 or less for surgery, Goal INR for neuraxial block anesthesia is 1.3 or less
- Re-check INR 12 hours after vitamin K dose
- Can proceed with surgery if INR 1.8 or less and patient can get FFP on the way to the OR (patient will receive GETA)
3. Clopidogrel, prasugrel, ticagrelor, cilostazol
- Continue any Acute Coronary Syndrome (treated medically or with stent) within last 12 months
- Continue if drug-eluding stent in last 6 months (in non-ACS)
- Continue if bare metal stent within last 1 month (in non-ACS)
- No need to delay surgery (patient will receive GETA)
4. Lovenox
- Hold before surgery
5. NOACs (dibigatran, rivaroxaban, apixiban, edoxaban)
- Hold, record time of last dose taken clearly. Clearance dependent on renal function.
- Generally hip fracture surgery with general anesthesia only can be undertaken 24 hours after last dose for all medications and normal renal function (48 hours for Dabigatran and Apixiban and high risk of bleeding). Risks and benefits should be weighed by teams (ortho, medicine, geriatrics, and anesthesia) for delaying surgery more than 24 hours.
Bridging
Bridging therapy with heparin indicated if any of the very high-risk conditions below:
- Mechanical heart valve
- Mitral prosthesis
- Caged ball/tilting aortic prosthesis
- Stroke/TIA within 6 months
- Atrial Fibrillation
- CHADS-VASC score 7-9 + absence of additional bleeding risk
- Stroke/TIA or systolic embolism within 3 months
- VTE
- VTE within 3 months
- Severe thrombophilia
- History of VTE during discontinuation of anticoagulation
Anesthesia
Contraindications or neuraxial + regional anethesia
1. GETA for patients with INR > 1.3 but able to go to surgery otherwise
2. Standard Preoperative antibiotics as a weight-based dose of Cefazolin
- Vancomycin for Cephalosporin allergic patients
- Vancomycin for penicillin allergic patients if the allergy was anaphylaxis
3. Tranexemic Acid 10mg/kg IV at the beginning and end of the case
- Any specific concerns for contraindications to be discussed between attendings
Cardiac Anesthesia
Only a requirement at the discretion of the anesthesia service (Medicine, Cardiology, or Geriatrics should NOT recommend)
Surgery
Coverage
- The Trauma Attending of the Day covers the case from 1PM until 7PM start time
- If the case can go after 7PM the general on-call attending covers
- If the case requires a total hip arthroplasty the arthroplasty attending on call or arthroplasty fellow will cover depending on availability.
- If the on-call attending or fellow is not available and the case can go then any arthroplasty faculty available will cover.
Standard Preoperative antibiotics as a weight-based dose of Cefazolin
Vancomycin for Cephalosporin allergic patients
Vancomycin for penicillin allergic patients if the allergy was anaphylaxis
Tranexemic Acid 10mg/kg IV at the beginning and end of the case
INR 1.5-1.8, give one unit FFP on call to OR
Hip Fracture Booking (only book with these codes)
- All cases that will be going for ORIF will be booked as: HIP FRACTURE ORIF (HIPT3045)
- All cases that will be going for CRPP will be booked as HIP FRACTURE CRPP (HIPT3205)
- All cases requiring a Hemiarthroplasty or Total Hip Arthroplasty will be booked as: HIP FRACTURE HEMIARTHROPLASTY (HIPT3044)
- In order to search for the appropriate booking code type in the alias “thundercat” and the three above codes will appear.
Pain control
1, Tylenol 1000mg TID ATC (IV ok if pt unable to take po); 650mg po TID if liver problems
2, As needed medications:
- If age>70, start Oxycodone 2.5mg po Q 3 hours prn, Dilaudid 0.4mg Q2 hour prn severe pain
- If age<70, start Oxycodone 5mg po Q 3 hours prn, Dilaudid 0.6 mg Q2 hours prn severe pain
3. Avoid Fentanyl (short-acting), gabapentin (sedating and increased risk of opioid overdose), use cold packs.
4. Pre-operative Fascia Iliaca block by ED provider or Acute pain service
Policy for Regional Anesthesia and Pain Control for Acute Hip Fractures in the ED
All patients with hip fractures should receive timely, effective, multi-modal analgesia. As part of this the Departments of Anesthesia and Perioperative Care, Emergency Medicine, Orthopedic Surgery recommend all patients receive an ultrasound-guided fascia iliaca block (FIB) as soon as appropriate and possible as this has been shown to decrease pain, need for opioids, and assist in timely transfer to OR.
- If the APS or regional anesthesia team is able to perform the procedure within 2 hours (Mon-Fri, 8am-5pm), then the ED will request placement of a FIB catheter (or one-time FIB, at discretion of APS or Regional Anesthesia team performing the block).
- If a catheter is placed, the APS or Regional Anesthesia team will administer a one-time dose of anesthetic; continuous infusions of anesthetic will only be done once the patient is admitted to an appropriate inpatient unit
- If the APS cannot respond within a reasonable amount of time (outside of Mon-Fri, 8am-5pm; or if APS team is otherwise unavailable), then the ED provider should proceed to performing a one-time FIB (or placement of a catheter, at discretion of ED provider).
- During off hours, the APS may consider requesting assistance from the E1, as appropriate and notifying the ED provider if an Anesthesia provider can respond urgently
- If the APS cannot respond urgently and the ED provider cannot perform the FIB, then the APS will collect the patient’s information and perform a timely consultation at the earliest opportunity to assess ongoing need for FIB. The APS consult will normally not come in from home during weekends or evenings/overnights specifically to perform the procedure.
- If a FIB catheter is placed, then the APS will follow the patient as a consult service.
Note: The FIB should be performed after call to the Orthopedic Surgery consult resident. While it is preferred that the consult resident evaluate the patient prior to or during FIB being performed, the ED or APS teams should proceed to performing the block as quickly as possible in the event of a delay to Orthopedic consultation. Unless there are specific concerns, the FIB should not be delayed until the patient is staffed with or evaluated by the Orthopedic Surgery senior resident or attending physician.
Fascia Iliaca Block Procedure/Protocol:
Contraindications to FIB:
- Coagulopathy or anticoagulant use, refer to: https://anesthesia.ucsf.edu/clinical-resources/guidelines-use-antithrombotic-agents-setting-neuraxial-procedures
- Allergy to local anesthetic
- Pre-existing peripheral neuropathy/neuromuscular disease or neuropathy as a result of trauma/injury
- Combative patients or any scenario where the block cannot be performed safely
- Signs of infection overlying injection site
Equipment
1. Order in Apex (medications are not stocked in block cart):
- Ropivacaine 0.2% 40cc OR Ropivacaine 0.5% 20cc + NS 20cc
- Lidocaine 1% 10cc (for skin infiltration)
2. Point-of-care ultrasound with high-frequency linear transducer Chlorhexidine swab
3. Ultrasound probe cover
4. Sterile gloves
5. From block cart:
- Block needle
- 20cc syringe x 2, 3-way stop-cock
- Needles/syringes for drawing up meds and performing skin infiltration
Management of Local Anesthetic Systemic Toxicity:
Protocol based on American Society for Regional Anesthesia and Pain Medicine: Checklist for Treatment of Local Anesthetic Systemic Toxicity
Call for Code Team
- Ventilate with 100% oxygen; prepare for intubation.
- Administer benzodiazepines for seizure activity.
- Initiate ACLS, if necessary.
AVOID vasopressin, calcium channel blockers, beta-blockers, or local anesthetic
REDUCE individual epinephrine doses to <1 mcg/kg - Administer 20% lipid emulsion therapy (Intralipid 20%).
- 1.5 cc/kg bolus over 1 min, followed by 0.25 cc/kg/min infusion
Repeat bolus every 5 min if hemodynamic instability persists; max 3 doses - May increase infusion to 0.5 cc/kg/min (max 10 cc/kg in first 30 mins of treatment)
- Continue infusion for at least 10 mins after return of hemodynamic stability
Additional considerations:
- Consider ECMO/cardiopulmonary bypass
- Prolonged CPR (>60 min) may be necessary
- AVOID: propofol, vasopressin, calcium channel blockers, beta-blockers, and lidocaine
- Consider amiodarone first line for arrhythmias
- After resuscitation, transfer patients to ICU for observation
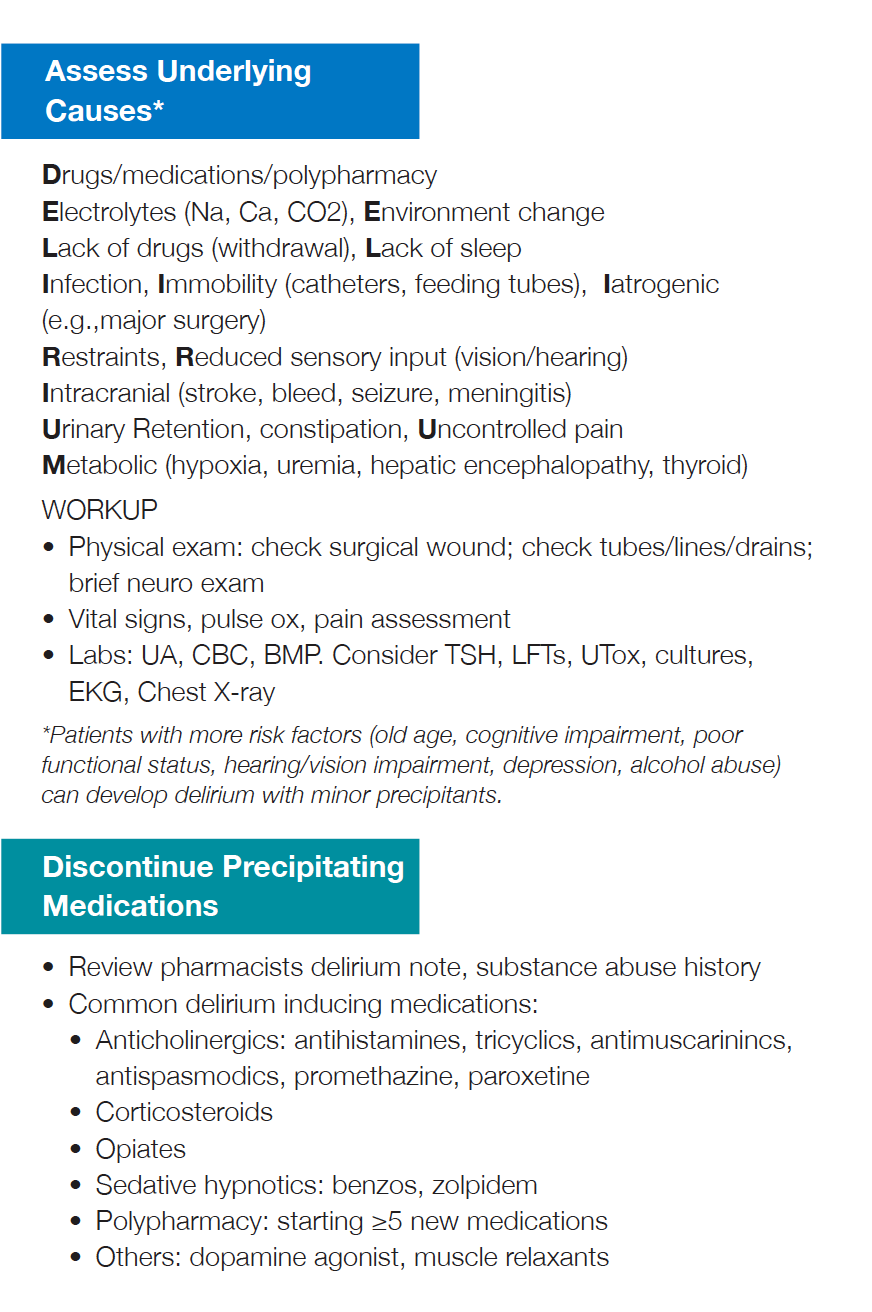
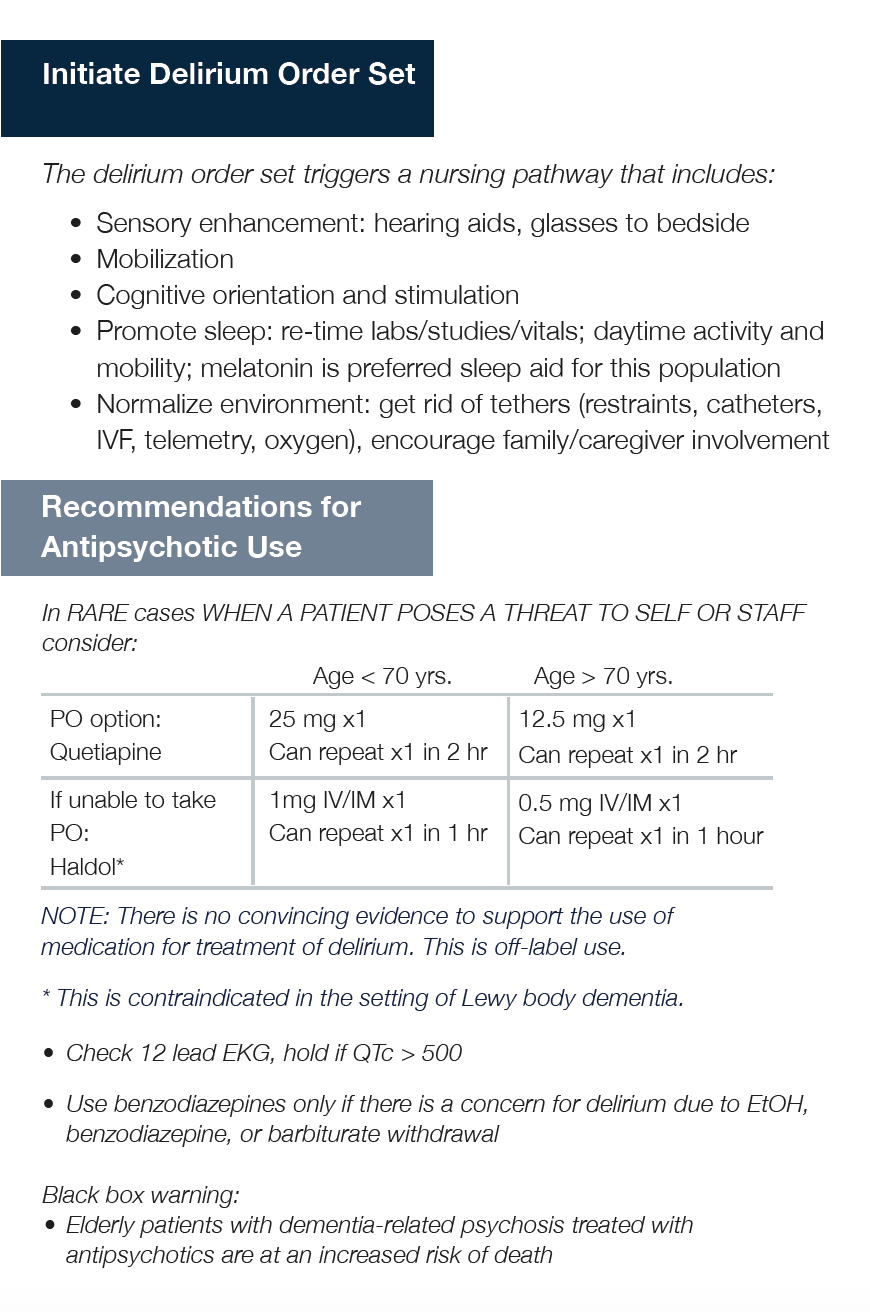
Delirium prevention/mangagement
1. Assess Underlying Causes
2. Discontinue preciptating medications
3. Iniitate delirium orderset
4. Use non-pharmacolgic treatment, medications have not been shown to treat or prevent delirium.
Post-op management and DVT prophylaxis
DVT prophylaxis: start POD #1
- For CrCl>31: Enoxaparin 40mg SQ x 4 weeks
- For CrCl<30: Aspirin 81mg BID x 4 weeks
Delirium prevention and order set (see link)
Patient seen by PT/OT in AM POD #1
Foley out POD #1, bladder scan straight cath if retention
Goal discharge to home or facility is < 48 hours
Osteoporosis management
- Start Calcium Carbonate 1250mg daily on discharge (alternatively can order extra strength Tums twice daily)
- Check Vit D level. If level is:
- < 15 then 50,000 IU weekly x 8 weeks then 2000IU daily
- 15-30 ---> start 2000IU daily
- 31-40 ---> 1000IU daily
- >40---> no supplementation needed
- Ask patient if they are followed by an osteoporosis or bone health specialist. If not, place a referral to orthopaedics and select skeletal health clinic.
- Add osteoporosis to the patient's problem list
- Educate patient on decreasing caffeine and alcohol intake, and smoking cessation
Discharge planning and follow up
3 appointments need to be made on discharge:
1. Orthopedics: Orthopedics Team schedules Orthopedic Surgery Follow up (based on surgical type)
a. ORIF: follow-up in Trauma Clinic with Advanced Health Provider for first visit
-
- Referral and Orthopedic Intern emails Orthopedic Institute Scheduling Desk for Trauma Clinic follow-up in 2 weeks with radiographs
b. Hemiarthroplasty or total hip arthroplasty: follow-up with Arthroplasty Fellow for first visit
-
- Referral and Orthopedic Intern emails Orthopedic Institute Scheduling Desk for Arthroplasty Fellow Clinic follow-up in 2 weeks with radiographs
- c. Non-Local patient: follow-up with a local orthopedic surgeon in 2 weeks with radiographs
2. Osteoporosis Management: If PCP not able to be contacted or to manage osteoporosis, Geriatrics or medicine consult places 'referral to orthopaedics-skeletal health' for follow up 1-2 months after discharge.'
3. Primary Care: Primary Team makes appointment with PCP within 2-4 weeks
a. Call the practice to arrange for the hospital f/u visit
b. Ortho-bundled payment program: If patient meets criteria for the OBP, a Care Support Program Nurse Practitioner will connect with patient before discharge to ensure continuity
c. Inpatient Case Manager & OBP Program Coordinator will be in communication to ensure collaboration with the UCSF complex care management team
d. NP from Care Support will often meet patient in house before discharge
Primary team ensures detailed instructions in the AVS:
- UCSF follow-up visits scheduled & listed with clinic addresses and phone numbers
- PCP
- Skeletal Health
- Orthopedic Surgery
- Post-op instructions
- Wound care/dressing changes
- Weight-bearing status
- DME
- Home Health orders
- Return precautions
- Specific instructions on when to call the doctor (PCP vs Orthopedic Surgeon)
- Updated Medication list
- DVT prophylaxis plan
Last Reviewed and Updated on 11/12/24